New Hampshire Medicaid provides health insurance coverage to over 176,000 Granite Staters, which is thirteen percent of the state's population.1 This includes children, pregnant women, people with disabilities, veterans, and older adults. Medicaid helps provide for everything from routine checkups and heart surgeries to cancer treatments and at-home nursing care. It covers prescriptions, mental health services, emergency care, dental and vision services, and substance use treatment. New Hampshire's Medicaid expansion program, called the Granite Advantage Health Care Program, is a unique solution that ensures working-age adults have access to health insurance. This program covered an average of nearly 58,000 individuals in 20251 and is the state's best tool in the fight against the ongoing substance use and mental health crises.
As a state, we must protect these vital programs that help all our residents get the health care they need.
Take Action
Share Your Story
Please share your experience with Medicaid programs, including Medicaid Expansion, using the form below. Tell us how the upcoming changes will impact you or a loved one, people in your communities, or your work.
- If you or a loved one are enrolled in Medicaid, how has it impacted your access to health care?
- How will the new reporting requirements (like being required to work or engage in community service for 80 hours/month) impact your ability to stay covered?
- If you were to lose your Medicaid coverage due to the new rules, how would it affect your health and daily life?
- If you have professional or other personal experience with Medicaid, how do you expect these changes to affect access to care in your workplace or community? What barriers are your patients, employees, or community members facing?
Spread the Word: Fact Sheet
Need help? Contact Wendy Chase (Community Engagement Coordinator) for help taking action or Sam Burgess (Health Care Policy Director) with policy questions.
About the Law
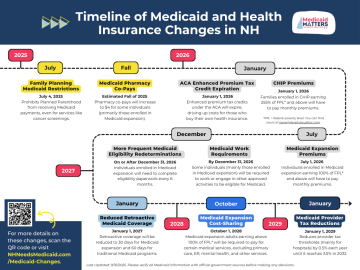
New requirements and costs are coming to New Hampshire’s Medicaid programs due to the 2026-27 NH state budget and a federal law known as the One Big Beautiful Bill Act. Changes include new work requirements, new monthly costs known as premiums and more frequent eligibility checks for some enrollees, and provider tax reductions, among other provisions. The changes will be implemented on specific dates in the coming months and years. Visit the NH Medicaid Matters website to learn more about the provisions and view the timeline.
The Consequences of Work Requirements
National data shows that the majority of adult Medicaid enrollees are already working. In 2023, 64% of adults covered by Medicaid were working full- or part-time. Of those not working, the top reasons reported were caregiving responsibilities, illness or disability, or school attendance. Only 8% of Medicaid adults reported they were retired, unable to find work, or not working due to other reasons.2
Work requirements pose a number of problems. They cause:
- Barriers to employment: Medicaid Expansion supports employment and our state's workforce by helping people get back to work. Access to necessary health care keeps people healthy and working, while losing health coverage makes it more difficult to manage health conditions necessary for maintaining employment.
- Gaps in coverage: When New Hampshire attempted to enforce work requirements in 2019, approximately 17,000 residents risked losing coverage.3 When Arkansas initiated work requirements in 2018, about one in four enrollees, which was more than 18,000 individuals, lost their coverage within the first 7 months.4 Losing health coverage can cause gaps in care, leaving people without any options for health coverage.
- Administrative burdens: Work requirements add an administrative burden that is costly and difficult to implement. Many eligible individuals face barriers to compliance, such as difficulty proving work status and reporting qualifying activities.3
Medicaid Expansion's Impact in New Hampshire
Since its inception in 2014, Medicaid Expansion has helped hundreds of thousands of Granite Staters access health care services. Across the 2024 fiscal year, 92,583 New Hampshire residents were enrolled in Medicaid Expansion at some point during the year.5
MedEx Helps Residents Access Mental Health and Substance Use Services
This program is especially important for Granite State individuals in need of mental health care and substance use disorder treatment, with about one in three recipients accessing these services. More than 25,000 people received mental health treatment and nearly 7,500 people accessed substance use disorder services in the last fiscal year.5 Medicaid Expansion makes a real difference, helping our residents receive the care they need to get healthy and contribute to their communities.
MedEx Increases Access to Care in Rural Regions of NH
Medicaid Expansion enrollment rates are higher in rural regions of New Hampshire, both increasing access to health care coverage in these communities and returning federal dollars to local economies.5, 6 This particularly benefits small, rural hospitals, helping them provide critical health services that could otherwise be difficult to access in these communities.6
MedEx Lowers Rate of Uninsured Residents
In the five years following Medicaid Expansion's inception in New Hampshire, the number of residents without health coverage declined. This drop was approximately 58,000 individuals, which is a 42.3% decline in the number of Granite Staters without health coverage.6
Law Status
On June 27, Governor Ayotte signed the state budget bills, HB 1 and HB 2, into law. Unfortunately, the budget bills include funding to implement work requirements for Medicaid expansion recipients, along with premiums and increased cost-sharing for some adults and children covered by Medicaid expansion and the Children’s Health Insurance Program (CHIP). Read statements from New Futures and other members of the NH Medicaid Matters Coalition on these changes to New Hampshire's Medicaid programs. New Futures is disappointed that these harmful provisions were included in the State Budget, and we vow to continue to work with our health care providers and our lawmakers to ensure that everyone in our state can access the health care they need.
To learn more about how a bill becomes a law, visit our About the Legislature webpage sign up for a New Futures advocacy training.
References
- New Hampshire Department of Health and Human Services, Division of Program Quality and Integrity. (2025, December 9). New Hampshire Medicaid Enrollment Demographic Trends and Geography. Retrieved December 29, 2025 from https://www.dhhs.nh.gov/sites/g/files/ehbemt476/files/documents2/bpq-da-medicaid-enrollment.pdf.
- Tolbert, J., Cervantes, S., Rudowitz, R., & Burns, A. (2025, May 30). Understanding the Intersection of Medicaid and Work: An Update. KFF. https://www.kff.org/medicaid/understanding-the-intersection-of-medicaid-and-work-an-update.
- Porter, J., Hodder, L., & LaRochelle, L. (2020, May). The Community Response to Medicaid Work and Community Engagement Requirements: Lessons from New Hampshire. University of New Hampshire Institute for Health Policy and Practice.
- Rudowitz, R., Musumeci, M., & Hall, C. (2025, August 9). February state data for Medicaid work requirements in Arkansas. KFF. https://www.kff.org/medicaid/state-data-for-medicaid-work-requirements-in-arkansas.
- State of New Hampshire Department of Health and Human Services, Office of the Commissioner. (2024, October 2). Granite Advantage Health Care Trust Fund, SFY 2024 Activities and Operations. Retrieved December 29, 2025 from https://gc.nh.gov/lba/Budget/FiscalItems/2024-10-18_Agenda_Items/FIS_24-364.pdf.
- New Hampshire Fiscal Policy Institute. (2023, January 17). The Effects of Medicaid Expansion in New Hampshire. https://nhfpi.org/resource/the-effects-of-medicaid-expansion-in-new-hampshire.