State Budget Impacts on NH's Children's Mental Health System
CONCORD, NH – On Wednesday, June 11, as New Hampshire lawmakers enter the final phases of developing their 2026-27 State Budget proposal, health care leaders and families with lived experience gathered to discuss the potential impacts of the budget on mental health services across the Granite State.
“Right now, more than 30% of young people in our state live with a diagnosed emotional or behavioral health condition,” Michele Merritt, President of New Futures, said at Wednesday’s press conference. “When their needs escalate, families often have nowhere to turn. Children are left boarding in emergency departments for days, sometimes weeks, waiting for psychiatric care. That’s not treatment—it’s trauma. And it’s unsustainable.”
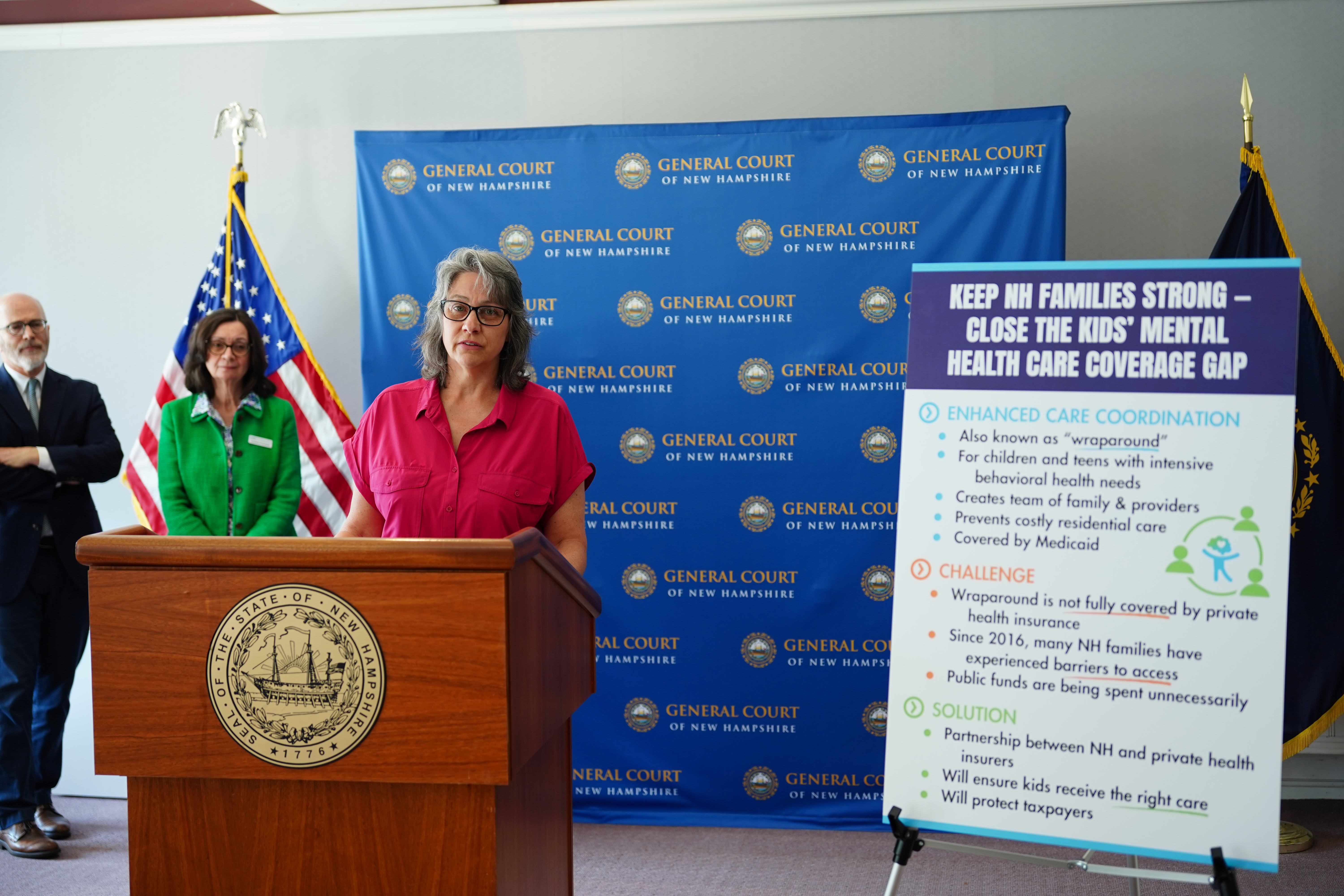
The Senate budget proposal, passed last week, includes stronger insurance coverage for children’s care coordination services, which will help further address the state’s emergency boarding crisis and ensure access to mental health care for Granite Staters in need.
“An investment in children’s mental health is one of the greatest investments we can make,” said Dennis Calcutt, Director of NH Connected Families. “This type of care coordination is critical and cannot wait. The best comparison I can make is that a child with a serious mental challenge and one with cancer have similar outcomes when proper care is not provided.”
The budget proposal is now entering its final phase, in which assigned members of the N.H. Senate and N.H. House of Representatives will work together on a Committee of Conference to resolve differences between the Senate-passed and House-passed spending plans. The Senate-passed version of the budget includes Senate Bill 128.
At Wednesday’s press conference, impacted families joined speakers from NAMI New Hampshire, Connected Families NH, and New Futures, to reiterate the critical need for this bill.
FAST Forward provides families with coordinated, evidence-based care that keeps children out of hospitals and in their homes. It includes not just clinical treatment, but also essential wraparound supports like care coordination, peer support, and family engagement. In New Hampshire, the state’s Medicaid program reimburses for FAST Forward, but commercial insurers refuse to cover the services.
“Last year, the state paid $1.9 million so that children with private insurance could access the FAST Forward wraparound program,” said Susan Stearns, Executive Director of NAMI New Hampshire. “As an employer, health insurance is one of our largest expenses, as it is for most employers. It seems more than reasonable that insurance carriers help pay for these essential mental health services.”
Lack of coverage for privately insured families is not an unfortunate oversight, but rather a clear attempt by insurers to avoid financial responsibility for treatment for their most vulnerable members.
“Insurance companies have a perverse financial incentive to delay or deny access to these services,” said Merritt. “Because when they do, the burden shifts to Medicaid—and to taxpayers. The system rewards commercial insurers for providing the least amount of care possible.”
Because private insurance companies currently do not cover FAST Forward wraparound services, families often have nowhere to turn for help when their child needs treatment.
“As a young child, my son struggled with anxiety. When he was 10 years old, he started running from school, eventually becoming unable to leave his bed,” said Cheryl Guerin, an Enfield parent. “I spent four years navigating NH’s systems seeking support and services. Our family faced an emergency room boarding and a stay at Hampstead Hospital.”
“Looking back, participation in the FAST Forward program was one of the key turning points in my son’s recovery and had the greatest impact on moving my family out of crisis,” added Guerin. “I’m proud to say that now, after receiving FAST Forward services, my son is doing very well. He has a 3.6 cumulative GPA with only a few credits to go on his high school diploma.”

