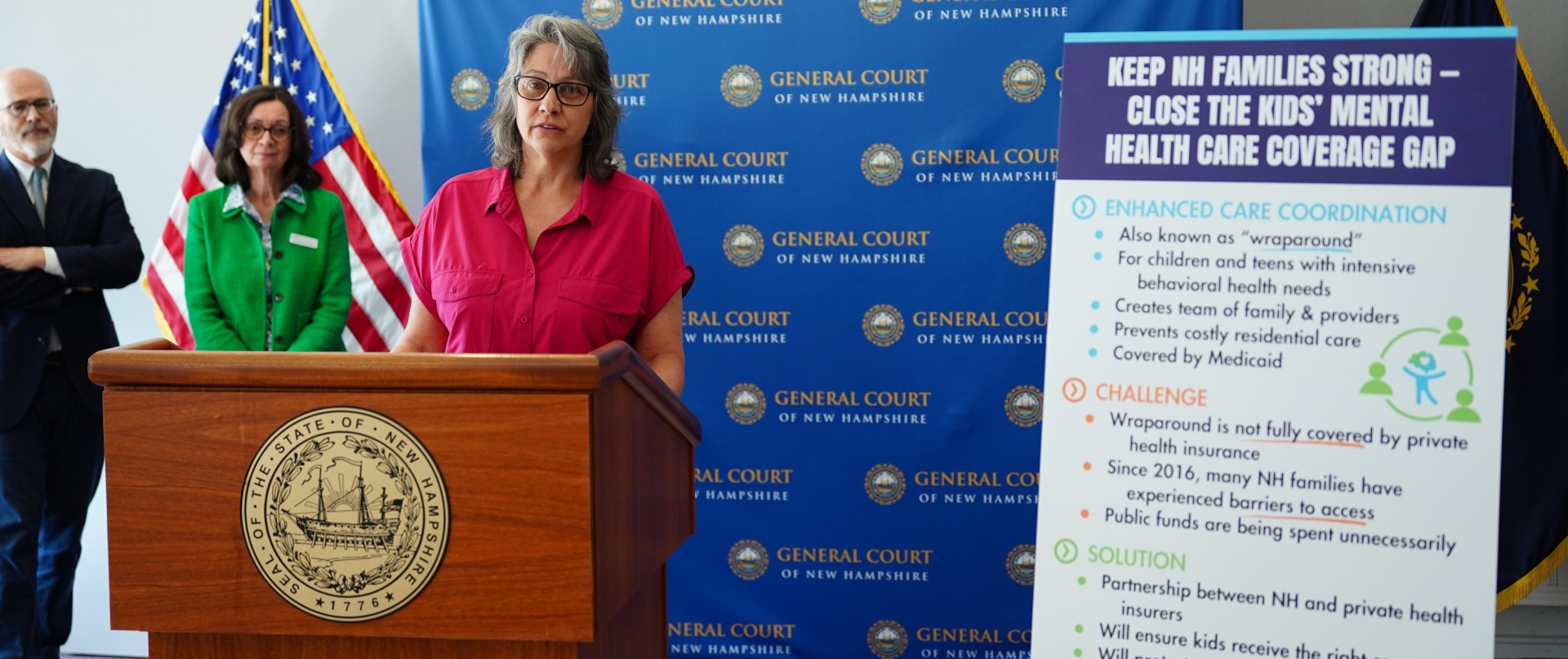
Enhanced care coordination programs, also called "wraparound," empower families caring for a child or teen with significant behavioral health needs, including mental health and substance use disorders.
Wraparound programs have helped hundreds of Granite State families navigate complex systems as they face a child's intensive behavioral health challenges. However, a private insurance coverage gap has created barriers for Granite State families and cost taxpayer dollars unnecessarily.
Senate Bill 498 would help more Granite State families access the care they need, regardless of their insurance type.
Learn More about Wraparound Programs
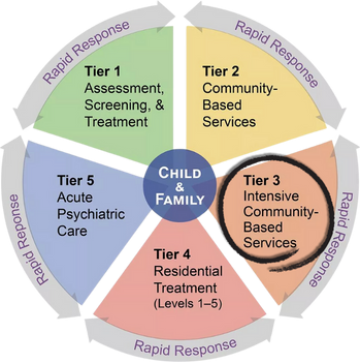
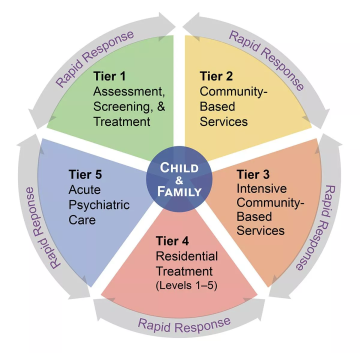
New Hampshire’s Children's System of Care for behavioral and mental health was designed with wraparound programs as its Tier 3 - Intensive, Community-Based Services. They are the Granite State's version of a proven youth- and family-centered planning and care coordination process.1 These programs serve families who have tried less intensive treatments and/or have complex situations requiring them to be involved in more than one “system” (e.g. juvenile justice, child protection, special education).
Wraparound programs help families clarify their strengths and needs. They then bring together a team to develop and implement a plan alongside them. The team can include the child, family, professional service providers, and other trusted adults.
There are three distinct wraparound programs in New Hampshire:
- FAST (Families and Systems Together) Forward wraparound for ages 5-21
- Early childhood wraparound for birth to 5
- Transitional Enhanced Care Coordination (TrECC) for youth in need of or transitioning out of residential treatment
Learn More About The Private Health Insurance Coverage Gap
While wraparound is included as part of Medicaid, it is unfortunately not covered by private health insurance corporations. This means Granite State families who purchase health insurance through their employer or the marketplace face significant barriers or may not be able to access these critical services.
To ensure access, stopgap measures currently allow some acutely ill children to become eligible for Medicaid through a special program, but not until their mental health challenges become severe.
Other families have had their wraparound care covered with taxpayer general fund dollars.
These extra steps have unnecessarily delayed appropriate care for children and teens while their struggles intensified.
About the Bill
- Protect taxpayers by preventing state general funds from subsidizing private health insurance corporations.
- Require private health insurance companies to help pay for these mental health services, creating a partnership between public and private insurers.
- Allow Tier 3 of the Children’s System of Care to work as intended for the first time.
- Help New Hampshire children get needed care, no matter what type of insurance they have.
- Contribute to more Granite State children and youth access the right care at the right time.
Take Action
Easy Email Template to Contact Your State Senator
Share Your Story
Will you share your experience to help support insurance coverage for enhanced care coordination in NH? Stories are powerful tools that can be shared with lawmakers and the public to influence policy change. New Futures can help you develop effective ways to share your story.
- Have you, a loved one, a client/patient, etc. either benefitted from or struggled to access youth behavioral/mental health care?
- Do you have experience with enhanced care coordination, or "wraparound", also known as FAST (Families and Systems Together) Forward, early childhood wraparound, or Transitional Enhanced Care Coordination (TrECC)?
Print or Download to Share: Advocacy Brief
Attend or Testify at a Public Hearing
Make your voice heard by attending or testifying at a public hearing! New Futures can help you prepare remarks, find the committee room, and offer moral support at the hearing.
The Senate Health and Human Services Committee held a public hearing for SB 498 on February 11. However, the bill may have a future hearing.
Need help? Contact Wendy Chase (Community Engagement Coordinator) for help taking action or Emma Sevigny (Senior Policy Director, Children's Behavioral Health) with policy questions.
Bill Status
Thursday, March 5: The full Senate will have a chance to weigh in on the bill. Please see ways you can make your voice heard above in the Take Action section.
February 18: The committee voted 4-1 to recommend the bill as “ought to pass” to the full Senate, with Senators Regina Birdsell, Pat Long, Suzanne Prentiss, David Rochefort in favor of the bill, and Senator Kevin Avard opposed.
February 11: The Senate Health and Human Services Committee held a public hearing. We are incredibly grateful to the many advocates who were in attendance. There were even two articles in the Concord Monitor that highlighted advocate stories and the importance of this bill.
January 7, 2026: Senate Bill 498 was introduced and assigned to the Senate Health and Human Services Committee.
You can learn more about how New Hampshire's legislative process works on our About the Legislature webpage, or take one of our advocacy trainings.
If you'd like to hear about the bill's progress, you can sign up for automated updates from the NH Legislature here.